Hypermobility Ehlers-Danlos Syndrome (hEDS) and Hypermobility
Spectrum Disorder (HSD) are both conditions related to connective tissue
disorders, specifically characterized by joint hypermobility, joint instability,
and chronic pain. Joint hypermobility refers to the ability of joints to move
beyond the normal range of motion.
hEDS is considered a heritable disorder, meaning it can be passed down
through generations. It is one of several subtypes of Ehlers-Danlos
Syndrome (EDS), a group of genetic connective tissue disorders.
Individuals with hEDS often experience joint hypermobility, skin
hyperextensibility (stretchiness), and tissue fragility.
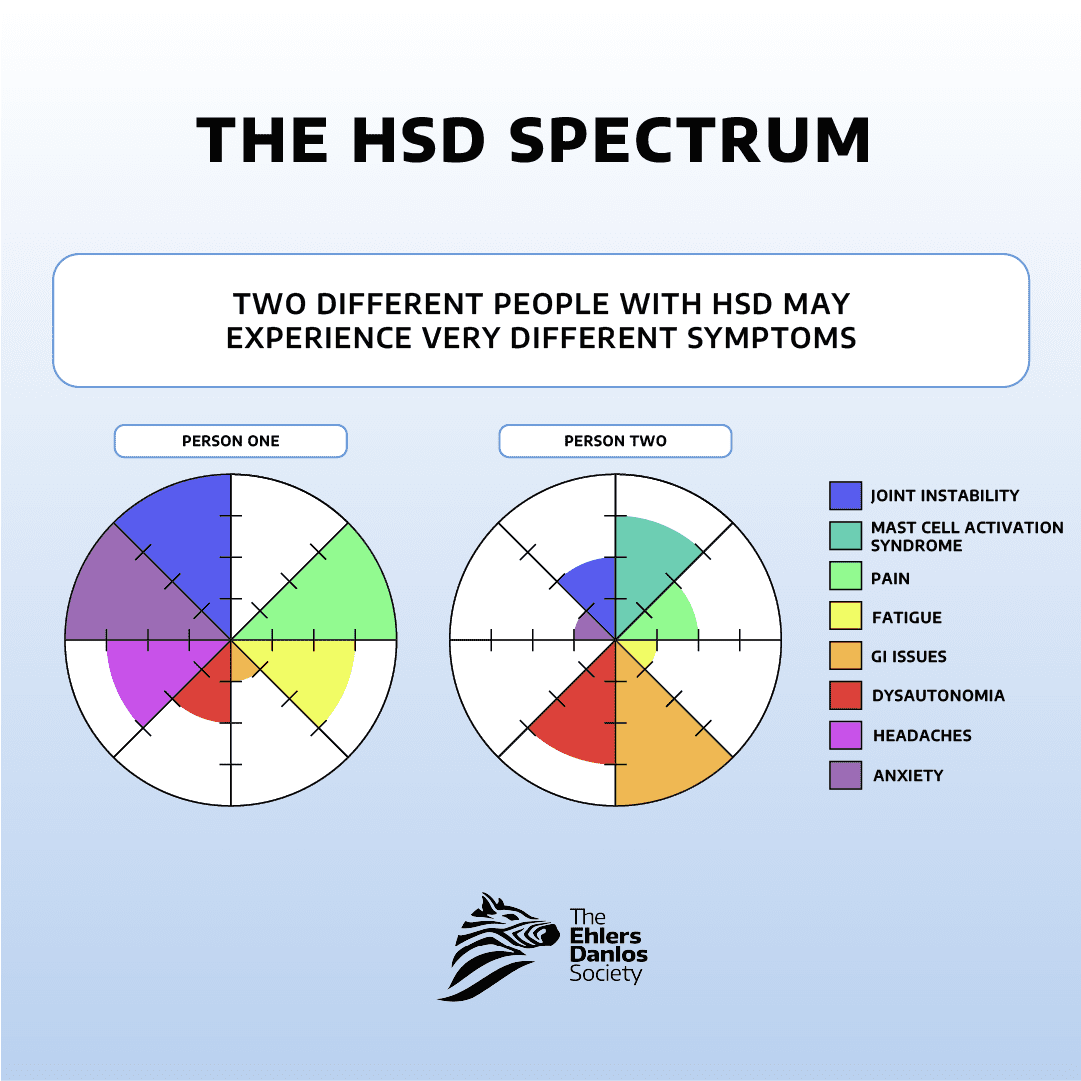
HSD, on the other hand, falls within the broader spectrum of hypermobility-related disorders. It
shares many features with hEDS but may not meet the specific diagnostic criteria for hEDS.
HSD is diagnosed when hypermobility-related symptoms are present but do not fully meet the
criteria for other types of EDS.

Both hEDS and HSD can manifest with a wide range of symptoms affecting various parts of the
body. These symptoms may include joint pain, fatigue, gastrointestinal issues, cardiovascular
problems, and more. Because of the diverse nature of symptoms, managing these conditions
often requires a multidisciplinary approach involving various healthcare providers, such as
rheumatologists, orthopedists, physical therapists, and pain specialists.
Fill out the form below and we will get back to you shortly on scheduling your appointment date!
CONTACT:
833-4 WE HEAL (833-493-4325)
FAX:
Virginia and Maryland: 833-918-2233
Florida: 888-803-9101
North Carolina: 833-849-9090
Email:
info@reenvisionpt.com
WORKING HOURS:
Monday – Friday
8:00AM – 5:00PM



Please note that the link will come from Phreesia, one of our partner companies.